The recent report by the French Court of Auditors on diabetes prevention and early care in France reveals critical gaps in national strategies, despite relatively modest progression rates. This analysis goes beyond national findings, synthesising the report with European and international research to offer a broader perspective on rising healthcare costs, persistent health inequalities, and the urgent need for robust preventive measures.
The valuable observations from the French authority serve to promote effective policies based on scientific evidence at EU level. Specific and easily implementable recommendations are highlighted, such as the mandatory adoption of Nutri-Score and the introduction of restrictions on the marketing of foods high in fat, sugar and salt (HFSS), as essential steps to reduce the significant burden of diabetes and promote health equity across Europe.
Introduction
Diabetes mellitus represents one of the defining health challenges of the 21st century, affecting over 10% of adults globally and imposing substantial economic burdens on healthcare systems (American Diabetes Association, 2024). The French Court of Auditors’ (Cour des Comptes) comprehensive report on diabetes prevention and early care provides a critical examination of France’s response to this epidemic, revealing both achievements and significant shortcomings in the nation’s approach to diabetes management and preventive care.
The report’s significance extends beyond France’s borders, offering valuable insights into the complexities of implementing effective diabetes prevention programmes within established healthcare systems. France’s experience illustrates the challenges faced by developed nations in balancing curative care with preventive interventions, particularly when addressing diseases that disproportionately affect vulnerable populations (Cour des Comptes, 2025).
Rising prevalence and economic burden
Demographic and economic pressures
The Court’s analysis reveals that while France’s diabetes progression rates remain relatively modest compared to international standards, the country faces mounting pressure from demographic transitions and associated healthcare costs. The report identifies population ageing as a primary driver of both increased diabetes prevalence and complications, creating a compound effect on healthcare expenditure (Cour des Comptes, 2025).
Current estimates suggest that diabetes prevalence in France stands at approximately 6% of the population, with the condition representing the highest prevalence among all chronic conditions covered by the nation’s statutory health insurance system (Bocquet et al., 2014). The Court’s findings indicate that healthcare costs attributable to diabetes continue to rise, primarily due to an expanding patient population and increasing numbers of individuals presenting with diabetes complications.
Healthcare expenditure trends
The economic burden of diabetes in France reflects broader international trends, with total costs encompassing both direct treatment expenses and indirect costs associated with complications. Previous research has documented that pharmacologically-treated diabetes patients in France incurred costs of €17.7 billion in 2010, including €2.5 billion directly related to diabetes treatment and prevention and €4.2 billion for complication management (Bocquet et al., 2014). The Court’s current analysis suggests these expenditures have continued to escalate, particularly in light of demographic pressures and the introduction of newer therapeutic interventions.
Health disparities and social determinants
Socioeconomic inequalities
The Court’s report emphasises that Type 2 diabetes disproportionately affects disadvantaged populations, with individuals in the lowest socioeconomic decile facing 2.8 times greater risk of developing the condition compared to those in the highest decile. This finding aligns with extensive international research demonstrating that social determinants of health play a crucial role in diabetes prevalence, management, and outcomes (Hill-Briggs et al., 2020).
The report’s identification of health disparities in diabetes care reflects broader patterns observed across developed nations, where racial, ethnic, and socioeconomic minorities experience higher rates of diabetes, poorer glycaemic control, and increased complications (Beckles & Chou, 2016). The Court’s emphasis on addressing these disparities through targeted public health interventions represents a critical component of comprehensive diabetes prevention strategies.
Geographical variations
Territorial inequalities in diabetes prevalence represent another significant finding, with overseas departments and regions demonstrating particularly high rates of the condition. This geographical variation mirrors patterns observed in other countries, where certain regions experience disproportionate diabetes burden due to combinations of environmental factors, limited healthcare access, and concentrated social disadvantage (Hill-Briggs et al., 2020).
The Court’s recognition of these geographical disparities underscores the need for tailored interventions that address local contexts and specific population needs. Research has consistently demonstrated that effective diabetes prevention programmes must account for community-specific factors, including cultural preferences, economic constraints, and healthcare infrastructure limitations (Galaviz et al., 2018).
Early detection and intervention challenges
Inadequate screening and detection
The report reveals that approximately 30% of individuals newly diagnosed with diabetes in 2021 presented with advanced disease, indicating significant failures in early detection and preventive screening. This finding has profound implications for both individual patient outcomes and healthcare system costs, as early intervention is associated with better glycaemic control and reduced complication rates (American Diabetes Association, 2024).
The Court identifies the ‘Mon bilan prévention’ programme, established by the 2023 Social Security Financing Law and generalised since summer 2024, as a potential solution for more systematic and targeted screening of at-risk populations. This initiative represents France’s attempt to implement comprehensive health screening that could facilitate earlier diabetes detection and intervention.
Existing support systems
The report acknowledges several existing care pathways and support systems, including the Sophia distance support service provided by health insurance, the Asalée nursing association programme, and therapeutic education programmes funded by regional health agencies. However, the Court suggests that these initiatives lack coordination and equitable access, limiting their effectiveness in addressing the diverse needs of diabetes patients.
Therapeutic education and adapted physical activity programmes represent core components of effective diabetes care, yet the report indicates that access to these services remains inconsistent across different populations and regions. The Court’s recommendation for integrated care pathways that include both therapeutic education and physical activity support reflects evidence-based approaches to diabetes management (Rosenfeld et al., 2024).
Lifestyle interventions and behavioural change
Evidence base for lifestyle modifications
The Court’s focus on lifestyle interventions aligns with the extensive body of research demonstrating their effectiveness in diabetes prevention. Scientific evidence has shown that:
- lifestyle interventions addressing diet, physical activity and behavioural change can lead to significant improvements in glycaemic control and reduce the risk of diabetes progression;
- comprehensive lifestyle programmes can reduce the incidence of type 2 diabetes by 25–58% among high-risk populations (Galaviz et al., 2018; Haw et al., 2017).
Implementation challenges
The Court’s analysis reveals significant gaps between evidence-based recommendations and real-world implementation of lifestyle modification programmes. The report suggests that current approaches lack the systematic structure and patient-centred design necessary for optimal effectiveness. This observation aligns with research indicating that successful diabetes prevention programmes require intensive, multi-component interventions delivered over extended periods.
Digital health interventions and eHealth platforms represent promising approaches to scaling lifestyle intervention programmes, with research demonstrating comparable effectiveness to traditional face-to-face delivery methods. The Court’s implicit recognition of the need for innovative delivery mechanisms reflects broader trends towards technology-enabled healthcare delivery.
Addressing social determinants and environmental factors
Nutritional policy and food environment
The Court’s recommendations for addressing nutritional determinants of diabetes risk represent a crucial component of comprehensive prevention strategies. The report reiterates findings from the Court’s 2019 obesity prevention analysis, emphasising the need for more stringent regulatory approaches to food marketing, nutritional labelling, and taxation policies affecting unhealthy food products.
The Court’s criticism of voluntary industry compliance mechanisms reflects evidence suggesting that regulatory interventions are more effective than voluntary approaches in promoting healthier food environments. Research has demonstrated that fiscal policies, including taxes on sugar-sweetened beverages and subsidies for healthy foods, can significantly influence dietary behaviours and diabetes risk (Rogers et al., 2024).
Comprehensive prevention strategies
The report’s recommendation for expanded restrictions on food advertising and enhanced behavioural taxation aligns with international best practices in diabetes prevention. The Court specifically suggests extending advertising restrictions to social media platforms and implementing policies to encourage reduced sugar content in food products. These recommendations reflect evidence-based approaches to creating supportive environments for healthy lifestyle choices.
Environmental interventions that address the broader context of diabetes risk factors have demonstrated effectiveness in reducing disease burden at population levels. The Court’s recognition of the need for multi-sectoral approaches involving health, agriculture, and economic ministries reflects contemporary understanding of health in all policies frameworks (Hill-Briggs et al., 2020).
International perspectives and comparative analysis
Global trends in diabetes prevention
France’s experience with diabetes prevention challenges reflects broader international patterns, where healthcare systems struggle to balance treatment demands with preventive care investments. Research demonstrates similar challenges in healthcare systems worldwide, where evidence-based prevention programmes remain underutilised despite widespread availability.
Health disparities in diabetes care represent a global phenomenon, with racial, ethnic, and socioeconomic minorities experiencing disproportionate disease burden across different healthcare systems. The Court’s identification of these disparities in the French context aligns with international research demonstrating persistent inequities in diabetes outcomes.
Successful prevention models
International examples of successful diabetes prevention programmes provide valuable insights for improving French approaches. The Finnish Diabetes Prevention Study and the United States Diabetes Prevention Program have demonstrated that intensive lifestyle interventions can achieve substantial reductions in diabetes incidence among high-risk populations (Tuomilehto et al., 2001; Knowler et al., 2002).
Community-based interventions that integrate cultural factors and address social determinants have shown particular promise in reducing health disparities. Research has demonstrated that culturally adapted programmes incorporating family-centred approaches can achieve significant improvements in diabetes prevention outcomes across diverse populations.
Healthcare system integration and policy implications
Coordinated care approaches
The Court’s recommendation for integrated care pathways reflects evidence supporting coordinated care models in diabetes management. Research has demonstrated that systematic approaches incorporating primary care, specialist services, and community resources can improve patient outcomes and reduce healthcare costs (American Diabetes Association, 2024).
Chronic care models that emphasise patient self-management, provider education, and system-level support have shown effectiveness in improving diabetes outcomes across diverse populations. The Court’s recognition of the need for systematic integration of therapeutic education and physical activity support aligns with these evidence-based approaches to comprehensive diabetes care.
Policy recommendations and implementation
The Court’s specific recommendations for enhancing preventive care within the Long-Term Condition (ALD) framework represent important policy innovations. The proposal to include non-pharmaceutical care pathways within ALD coverage could significantly improve access to lifestyle interventions and therapeutic education services.
Payment system reforms that support preventive interventions represent crucial components of effective diabetes prevention strategies. Research has demonstrated that value-based payment models that reward prevention and early intervention can improve patient outcomes while reducing overall healthcare costs.
Technological innovation and future directions
Digital health solutions
The Court’s implicit recognition of the need for innovative delivery mechanisms aligns with growing evidence supporting digital health interventions in diabetes prevention. Research has demonstrated that mobile health applications, telehealth platforms, and remote monitoring systems can effectively deliver lifestyle interventions and support patient self-management.
Artificial intelligence and machine learning applications represent promising approaches to personalising diabetes prevention interventions and identifying high-risk individuals. The Court’s emphasis on systematic screening and targeted interventions could benefit from technological innovations that enhance risk stratification and personalised care approaches.
Precision medicine approaches
Emerging research in precision medicine offers opportunities to tailor diabetes prevention strategies based on individual genetic, environmental, and lifestyle factors. The Court’s recognition of the need for personalised care pathways reflects broader trends towards individualised healthcare approaches that could enhance intervention effectiveness.
Biomarker-based screening and predictive analytics represent areas of active research that could improve early detection and intervention targeting. The Court’s emphasis on systematic screening could benefit from technological advances that enhance diagnostic accuracy and risk prediction capabilities.
Economic considerations and cost-effectiveness
Investment in prevention
The Court’s findings regarding escalating healthcare costs underscore the economic imperative for investing in diabetes prevention. Research has consistently demonstrated that preventive interventions generate substantial return on investment through reduced treatment costs and improved productivity (Haw et al., 2017).
Cost-effectiveness analyses of diabetes prevention programmes have shown that intensive lifestyle interventions can achieve significant healthcare savings over extended periods. The Court’s recognition of the need for systematic prevention approaches reflects evidence supporting the economic value of upstream interventions in chronic disease management.
Healthcare system sustainability
The Court’s emphasis on healthcare system sustainability reflects broader concerns about the long-term viability of treatment-focused approaches to diabetes management. Research has demonstrated that prevention-oriented healthcare systems can achieve better population health outcomes while maintaining cost control (Rosenfeld et al., 2024).
Value-based healthcare models that emphasise population health outcomes rather than service volume represent promising approaches to sustainable diabetes care. The Court’s recommendations for systematic prevention approaches align with these innovative healthcare delivery models.
The diabetes epidemic in the European Union
The diabetes epidemic in the European Union presents a formidable public health challenge that demands urgent, coordinated action across all member states. Current estimates indicate that over 33 million adults in the EU are living with diabetes, with this figure projected to rise to 38 million by 2030 (European Commission, 2024). The WHO European Region reports that approximately 74 million adults (11.9% of men and 10.9% of women) are living with diabetes, representing the highest burden of Type 1 diabetes globally (WHO Europe, 2024).
Alarmingly, approximately one in three people living with diabetes in the EU are unaware of their condition, highlighting massive gaps in screening programmes and early detection systems.
The burden extends beyond individual health outcomes, with diabetes-related complications causing 686,000 deaths annually across the EU and imposing substantial economic costs on healthcare systems (Del Prato et al., 2024). Recent research demonstrates increasing Type 2 diabetes prevalence across all EU countries, with significant variations in disease burden between regions. This escalating disease burden disproportionately affects vulnerable populations and exacerbates existing health inequalities across European societies.
Tackling the diabetes challenge in the EU: a call to action
The urgent necessity to address this public health crisis necessitates the implementation of a comprehensive EU nutrition policy that transcends individual member state approaches and establishes harmonised standards for diabetes prevention. This policy must be based on a harmonised system of food classification in relation to their nutritional profiles – whose vanguard is today expressed by the algorithms underlying Nutri-Score.
On this basis, one must therefore proceed first and foremost, without further delay, to:
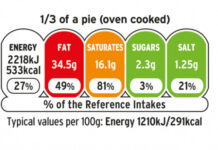
- introduce Nutri-Score as the harmonised Front-of-Pack Nutrition Labelling (FoPNL) system. This system is indeed the only one, amongst the various ones adopted thus far, to have achieved a significant level of diffusion across several EU member states. A level of diffusion that is indeed extraordinary, considering the unparalleled success of the Yuka app which bases its nutritional assessment of foods upon it. Nutri-Score, it is worth adding, is the FoPNL system with the broadest support from scientific literature and recognition from various international organisations (OECD, IARC, WHO, UNESCO);
- The mandatory adoption of Nutri-Score on all food packaging and fast-food menus across the EU must be prioritised. To date, the European Commission has failed to act on the legislative mandate to recognise Nutri-Score as the sole harmonised front-of-pack nutrition labelling system. This inaction continues to favour the private interests of corporations producing ultra-processed foods over the public health needs of the population (Julia et al., 2025). This situation must end. Scientific evidence has consistently demonstrated the effectiveness of Nutri-Score labelling in enabling consumers to make healthier food choices (Andreani et al., 2025) – an essential component of any equitable food policy;
- reform the Audiovisual Media Services Directive (AVMSD) to strengthen the protection of European citizens, starting with children and adolescents, against aggressive marketing of HFSS foods. The failure of the AVMSD – which is based on ‘self-regulation’ – has been recognised by the European Commission itself (2021),which however has not yet proposed its revision to this day. Norway meanwhile, as has been seen, has indicated the path to follow.
#Égalité!
Dario Dongo
Cover art copyright © 2025 Dario Dongo (AI-assisted creation)
References
- American Diabetes Association Professional Practice Committee. (2024). Introduction and methodology: Standards of care in diabetes – 2024. Diabetes Care, 47(Supplement_1), S1-S4. https://doi.org/10.2337/dc24-SINT
- Andreani, G., Sogari, G., Wongprawmas, R., Menozzi, D., & Mora, C. (2025). Nutri-Score and Eco-Score Labeling: A Systematic Review of Their Impact on Consumer Understanding, Attitudes, and Behaviors. Food Reviews International 1-25.https://doi.org/10.1080/87559129.2025.2460052
- Chevreul, K., Berg Brigham, K., & Bouché, C. (2014). The burden and treatment of diabetes in France. Globalization and Health, 10, Article 6. https://doi.org/10.1186/1744-8603-10-6
- Cour des Comptes, France (2025, July). Prévention et prise en charge précoce du diabète. Retrieved from https://www.ccomptes.fr/fr/publications/prevention-et-prise-en-charge-precoce-du-diabete
- Del Prato, S., Torbeyns, B., Mathieu, C., Kempler, P., Lalić, N. M., Nolan, J. J., Párniczky, A., & Roden, M. (2024). 2024: The year to take European action on diabetes to the next level. Diabetologia, 67(7), 1155-1158. https://doi.org/10.1007/s00125-024-06166-9
- European Commission. Diabetes. Retrieved 10 July 2025, from https://research-and-innovation.ec.europa.eu/research-area/health/diabetes_en
- Galaviz, K. I., Weber, M. B., Straus, A., Haw, J. S., Narayan, K. M. V., & Ali, M. K. (2018). Global Diabetes Prevention Interventions: A Systematic Review and Network Meta-analysis of the Real-World Impact on Incidence, Weight, and Glucose. Diabetes care, 41(7), 1526–1534. https://doi.org/10.2337/dc17-2222
- Haw, J. S., Galaviz, K. I., Straus, A. N., Kowalski, A. J., Magee, M. J., Weber, M. B., Wei, J., Narayan, K. M. V., & Ali, M. K. (2017). Long-term Sustainability of Diabetes Prevention Approaches: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA internal medicine, 177(12), 1808–1817. https://doi.org/10.1001/jamainternmed.2017.6040
- Hill-Briggs, F., Adler, N. E., Berkowitz, S. A., Chin, M. H., Gary-Webb, T. L., Navas-Acien, A., Thornton, P. L., & Haire-Joshu, D. (2020). Social Determinants of Health and Diabetes: A Scientific Review. Diabetes care, 44(1), 258–279. Advance online publication. https://doi.org/10.2337/dci20-0053
- Knowler, W. C., Barrett-Connor, E., Fowler, S. E., Hamman, R. F., Lachin, J. M., Walker, E. A., Nathan, D. M., & Diabetes Prevention Program Research Group (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England journal of medicine, 346(6), 393–403. https://doi.org/10.1056/NEJMoa012512
- Julia, C., Gokani, N., Hercberg, S., Garde, A., & Touvier, M. (2025). Ten years of Nutri-Score front-of-pack nutrition labelling in Europe. Nature Food, 6(3), 239–243. https://doi.org/10.1038/s43016-025-01141-y
- Rogers NT, Cummins S, Jones CP, et al., (2024). Estimated changes in free sugar consumption one year after the UK soft drinks industry levy came into force: controlled interrupted time series analysis of the National Diet and Nutrition Survey (2011–2019). J Epidemiol Community Health. 2024. DOI: 10.1136/jech-2023-221051
- Tuomilehto, J., Lindström, J., Eriksson, J. G., Valle, T. T., Hämäläinen, H., Ilanne-Parikka, P., Keinänen-Kiukaanniemi, S., Laakso, M., Louheranta, A., Rastas, M., Salminen, V., Uusitupa, M., & Finnish Diabetes Prevention Study Group (2001). Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. The New England journal of medicine, 344(18), 1343–1350. https://doi.org/10.1056/NEJM200105033441801
- UNESCO Chair GHE. (2023). Report: Why the European Commission must choose the Nutri-Score nutrition label. Retrieved from https://unescochair-ghe.org/2023/05/12/report-why-the-european-commission-must-choose-the-nutri-score-nutrition-label/
- WHO Europe. Diabetes. Retrieved 10 July 2025, from https://www.who.int/europe/health-topics/diabetes
Dario Dongo, lawyer and journalist, PhD in international food law, founder of WIISE (FARE - GIFT - Food Times) and Égalité.