Nickel allergy represents the most prevalent form of contact allergy worldwide, affecting approximately 8-19% of adults and 8-10% of children and adolescents in Europe, with a pronounced female predominance. This review examines the current understanding of nickel allergic contact dermatitis (Ni-ACD), its pathophysiology, diagnostic methodologies, clinical manifestations, and therapeutic approaches.
Despite the implementation of the European Nickel Directive 94/27/EC, which regulated the release of nickel from certain products to prevent allergic reactions, substantial challenges persist in managing this condition.
The emergence of systemic nickel allergy syndrome (SNAS) as a distinct clinical entity has further complicated the therapeutic landscape. This review synthesises evidence from recent epidemiological studies, advanced diagnostic techniques, and novel treatment strategies to provide clinicians with a contemporary understanding of nickel allergy management.
Introduction
Nickel (Ni) is a ubiquitous transition metal that serves as the leading cause of allergic contact dermatitis globally (Ahlström et al., 2019; Silverberg et al., 2024). The metal’s widespread industrial applications in jewellery, coins, electronic devices, and various consumer products ensure continuous human exposure, making nickel hypersensitivity a significant public health concern.
The clinical spectrum of nickel-induced allergic reactions ranges from localised contact dermatitis to systemic manifestations, including the recently recognised systemic nickel allergy syndrome (SNAS) (Lombardi et al., 2020; Conti et al., 2021).
The pathogenesis of nickel allergy involves a complex interplay of genetic predisposition, environmental exposure, and immunological mechanisms. Once nickel sensitisation occurs, individuals remain susceptible to allergic reactions throughout their lifetime, as the condition represents a permanent alteration of the immune system’s response to this metal allergen (Rishor-Olney & Gnugnoli, 2023).
Methodology
Review approach
This narrative review synthesises current knowledge on nickel allergy from contemporary literature published between 2019 and 2024. The review was conducted through web-based literature searches using terms including ‘nickel allergy’, ‘allergic contact dermatitis’, ‘systemic nickel allergy syndrome’, ‘patch testing nickel’, ‘nickel regulation’, and related terminology. Primary sources were accessed through academic databases and peer-reviewed publications to ensure scientific accuracy and clinical relevance.
Literature selection
Publications selected for inclusion comprised recent peer-reviewed articles, clinical guidelines, epidemiological studies, and regulatory assessments addressing various aspects of nickel allergy. Priority was given to high-impact journals and studies with robust methodological approaches. Contemporary research was emphasised to reflect current understanding and practice patterns in nickel allergy management.
Content synthesis
The review integrates findings across multiple domains, including epidemiology, pathophysiology, clinical manifestations, diagnostic approaches, treatment strategies, and prevention measures. Evidence synthesis was conducted thematically to provide comprehensive coverage of current knowledge whilst identifying areas requiring further research investigation.
Epidemiology and risk factors
Global prevalence
Nickel allergy prevalence demonstrates significant geographical and demographic variation. In European populations, the prevalence ranges from 8-19% in adults and 8-10% in children and adolescents, with a striking female predominance (Ahlström et al., 2019).
The North American Contact Dermatitis Group reported that 18.0% of tested individuals showed positive reactions to nickel sulfate hexahydrate, establishing it as the most frequent contact allergen (Silverberg et al., 2024).
Demographic patterns
Gender differences in nickel allergy prevalence are pronounced, with women showing approximately five times higher rates than men. This disparity primarily reflects differential exposure patterns, particularly through jewellery wearing and ear piercing practices.
The paediatric population demonstrates increasing sensitisation rates, with some studies reporting a four-fold increase in incidence over the past three decades (Silverberg et al., 2020).
Occupational exposure
Occupational nickel exposure remains a significant risk factor in multiple industries. Healthcare workers, particularly nurses, demonstrate elevated nickel sensitisation rates of 57.1% compared to other occupational groups, highlighting the importance of workplace exposure assessment (Greco et al., 2023). Manufacturing industries involving nickel-containing materials continue to pose substantial risks despite regulatory interventions.
Environmental factors
Environmental exposure patterns have evolved following regulatory changes. The implementation of the EU Nickel Directive 94/27/EC has resulted in measurable reductions in nickel allergy prevalence among young women in Denmark, Germany, Italy, and the United Kingdom (Garg et al., 2013).
However, consumer exposure to nickel through mobile phones, tablets and other electronic devices represents an emerging source of contact that should be considered within the framework of the General Product Safety Regulation (EU) No 2023/988 regime (Dongo, 2023).
Pathophysiology and immunological mechanisms
Sensitisation process
Nickel sensitisation follows classic Type IV hypersensitivity mechanisms, involving delayed-type hypersensitivity reactions mediated by T-lymphocytes. The process begins when nickel ions penetrate the skin barrier and bind to endogenous proteins, forming hapten-protein complexes that are recognised as foreign by the immune system (Ahlström et al., 2019).
Molecular mechanisms
Dendritic cells serve as primary antigen-presenting cells, capturing nickel-protein conjugates and presenting them to naive T-cells in regional lymph nodes.
This process involves major histocompatibility complex (MHC) class II molecules and requires appropriate costimulatory signals for effective T-cell activation.
Once activated, nickel-specific T-cells undergo clonal expansion and acquire memory phenotypes, ensuring rapid responses upon subsequent exposure.
Elicitation phase
Upon re-exposure, memory T-cells rapidly recognise nickel antigens and initiate inflammatory cascades:
- Th1-mediated responses predominate in acute reactions, whilst Th2 responses may contribute to chronic manifestations;
- inflammatory mediators including interleukin-2, interferon-gamma, and tumour necrosis factor-alpha orchestrate the characteristic inflammatory response observed in nickel contact dermatitis.
Systemic responses
Systemic nickel allergy syndrome represents a distinct pathophysiological entity where dietary nickel or nickel-containing implants trigger systemic immune responses.
The mechanisms underlying SNAS pathophysiology involve gastrointestinal absorption of nickel, followed by systemic circulation and subsequent immune activation in predisposed individuals.
Clinical manifestations
Localised contact dermatitis
Classic nickel dermatitis presents as erythematous, oedematous lesions at sites of direct contact with nickel-containing objects. Common locations include earlobes (from earrings), wrists (from watches), abdomen (from belt buckles), and fingers (from rings). The dermatitis pattern typically corresponds precisely to the contact area, facilitating clinical diagnosis.
Chronic hand eczema
Hand eczema represents a severe manifestation of nickel allergy, often resulting in chronic, disabling symptoms. The condition may present as dyshidrotic eczema, nummular eczema, or chronic dermatitis affecting palms, fingers, and dorsal hand surfaces. Quality of life impairment is substantial, with significant impacts on occupational functioning and daily activities.
Systemic Nickel Allergy Syndrome
SNAS encompasses a constellation of extra-cutaneous symptoms associated with systemic nickel exposure.
Clinical manifestations include gastrointestinal symptoms (abdominal pain, diarrhoea, nausea), respiratory symptoms (asthma, rhinitis), and systemic symptoms (headache, fatigue, joint pain) (Minelli et al., 2015).
The prevalence of SNAS has been estimated at 5.78% among patients undergoing allergy evaluation in specialised centres.
Implant-related reactions
Nickel-containing medical implants can trigger allergic reactions in sensitised individuals:
- orthopaedic implants, dental materials, and cardiac devices containing nickel may cause peri-implant dermatitis, implant loosening, or systemic symptoms;
- the diagnosis of implant allergy requires careful correlation between clinical symptoms and immunological testing.
Diagnostic methodologies
Patch testing
Patch testing remains the gold standard for diagnosing nickel allergy. The procedure involves applying nickel sulfate (2.5% in North America, 5% in Europe) to the upper back under occlusion for 48 hours, followed by reading at 72-96 hours.
Test interpretation follows International Contact Dermatitis Research Group criteria, with positive reactions graded from weak positive (+) to strong positive (+++) (Silverberg et al., 2024).
Technical considerations
Patch test reliability depends on multiple factors, including test concentration, vehicle selection, application site, and patient preparation. Recent studies have evaluated different nickel preparations and found that test sensitivity may be enhanced through site pretreatment or repeated testing in individuals with negative initial results but strong clinical suspicion.
Alternative testing methods
In vitro testing methods include the lymphocyte transformation test (LTT), which measures T-cell proliferation in response to nickel stimulation. The memory lymphocyte immunostimulation assay (MELISA) represents another in vitro approach, though its clinical utility remains controversial. Intradermal testing has been investigated but is not routinely recommended due to sensitisation risks.
Diagnostic challenges
False-negative results may occur in patients with active dermatitis, recent corticosteroid use, or inadequate test concentrations.
False-positive reactions can result from irritant responses or excited skin syndrome. Clinical correlation remains essential for accurate diagnosis establishment.
Treatment and management strategies
Avoidance measures
Primary treatment of nickel allergy involves the strict avoidance of nickel-containing products. This includes:
- jewellery selection, by opting for materials such as surgical-grade stainless steel, titanium, or gold;
- clothing modifications, such as avoiding metal fasteners, buttons or zips that may contain nickel;
-
occupational precautions, meaning the implementation of safety measures in workplaces where nickel exposure is common. For instance:
- hairdressers may need to avoid nickel-coated tools (e.g. scissors, clips) and use nickel-free alternatives;
- construction workers and mechanics should wear protective gloves to reduce skin contact with metal tools or machinery;
- healthcare professionals are advised to use nickel-safe medical instruments, such as stethoscopes or surgical tools.
In addition, consumer education on hidden sources of nickel — such as in electronic devices, cosmetics, and household items — is essential for effective prevention and management.
Topical therapies
Acute dermatitis responds well to topical corticosteroids ranging from medium-potency preparations for body sites to low-potency formulations for facial involvement. Calcineurin inhibitors (tacrolimus, pimecrolimus) provide steroid-sparing alternatives for chronic management, particularly in sensitive skin areas.
Systemic treatments
Severe generalised dermatitis may require systemic corticosteroids for acute control. Immunosuppressive agents, including methotrexate, azathioprine, and cyclosporine, have been employed for refractory hand eczema. Dupilumab, an IL-4/IL-13 receptor antagonist, has shown promise in atopic dermatitis with nickel sensitisation.
Emerging therapies
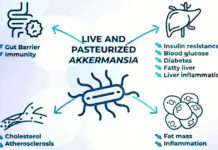
Oral immunotherapy for nickel allergy has been investigated in European studies, showing promising results for SNAS management:
- low-dose immunotherapy and sublingual desensitisation represent experimental approaches requiring further clinical validation;
- probiotic interventions have been explored for SNAS treatment, with preliminary evidence suggesting symptom improvement through microbiome modulation (Lombardi et al., 2020; Randazzo et al., 2015).
SNAS-specific management
SNAS treatment primarily involves low-nickel dietary restrictions combined with symptomatic management:
- dietary guidance includes avoiding high-nickel foods such as chocolate, nuts, legumes (e.g., lentils, beans, peas), and certain vegetables including spinach, asparagus, and cabbage;
- nutritional counselling is essential to prevent dietary deficiencies during elimination protocols.
Prevention and regulatory approaches
European Nickel Directive
The European Nickel Directive 94/27/EC, incorporated into REACH Regulation (Entry 27, Annex XVII), established release limits for nickel-containing consumer products. The amended regulation limits nickel release to 0.5 μg/cm²/week for products in direct prolonged skin contact and 0.2 μg/cm²/week for post assemblies inserted through pierced body parts.
Regulatory impact assessment
Epidemiological studies have demonstrated significant reductions in nickel allergy prevalence following regulatory implementation.
Young women in Denmark, Germany, Italy, and the United Kingdom showed statistically significant decreases in nickel sensitisation rates, providing strong evidence for regulatory effectiveness (Garg et al., 2013).
Limitations of current regulations
Despite regulatory success, challenges persist in nickel exposure control. Electronic devices, mobile phones, and tablets often exceed release limits, representing emerging exposure sources. Occupational exposures remain inadequately regulated, and enforcement mechanisms require strengthening.
Regulation (EU) 2024/1987: nickel in foodstuffs
Regulation (EU) 2024/1987 intervenes to amend the food contaminants regulation (EU) 2023/915 to introduce at the European level the first harmonised nickel limits in foods.
It defines specific limits in 16 food categories including cereals, chocolate and infant formulas — main sources of nickel in the diet — based on the most recent risk assessments conducted by EFSA.
The measure has particular relevance because it recognises systemic nickel exposure as a public health problem, particularly in the management of SNAS. It applies from 1 July 2025, one year later for cereals.
Major outcomes and clinical significance
Public health impact
Nickel allergy represents a substantial public health burden with significant socioeconomic implications. Healthcare costs associated with chronic dermatitis, occupational disability, and quality of life impairment justify continued prevention efforts. Paediatric nickel sensitisation has lifelong consequences, emphasising the importance of early prevention strategies.
Quality of life considerations
Chronic nickel dermatitis significantly impacts psychological well-being, social functioning, and occupational performance:
- hand eczema associated with nickel allergy can result in career limitations and functional disability;
- SNAS patients often experience chronic fatigue, gastrointestinal disturbance, and reduced quality of life.
Treatment outcomes
Conservative management through allergen avoidance remains highly effective when rigorously implemented.
Topical therapies provide adequate symptom control in most patients with localised dermatitis.
Systemic treatments show variable efficacy for severe disease, with novel biologics and probiotics offering promising alternatives.
Long-term prognosis
Nickel allergy represents a permanent condition with no spontaneous resolution. Long-term studies indicate that consistent avoidance can lead to symptom remission, though re-exposure invariably triggers allergic reactions. SNAS patients may achieve symptom improvement through dietary modifications and comprehensive management approaches.
Interim conclusions
Nickel allergy remains the most prevalent contact allergy worldwide, affecting millions of individuals with significant morbidity. The pathophysiology involves complex immunological mechanisms resulting in delayed-type hypersensitivity with potential systemic manifestations. Diagnostic methodologies centre on patch testing, though emerging techniques may enhance diagnostic accuracy.
Treatment strategies primarily rely on allergen avoidance, supplemented by topical and systemic therapies for symptom management. The recognition of SNAS as a distinct clinical entity has expanded therapeutic considerations to include dietary modifications and novel immunotherapeutic approaches.
Regulatory interventions, particularly the Nickel Directive 94/27/EC and the recent Commission Regulation (EU) 2024/1987 addressing dietary nickel limits, have demonstrated measurable success in reducing nickel allergy prevalence and providing frameworks for systematic exposure control. However, evolving exposure patterns through electronic devices and persistent occupational hazards require continued vigilance and potential regulatory updates.
Future research priorities include developing more effective treatments for severe disease, optimising diagnostic techniques, and addressing emerging exposure sources. Prevention strategies must evolve to encompass modern lifestyle exposures whilst maintaining the gains achieved through existing regulatory frameworks.
The global burden of nickel allergy underscores the need for continued research, improved prevention strategies, and enhanced clinical management approaches. International cooperation in regulatory harmonisation and research collaboration will be essential for reducing the incidence and impact of this prevalent allergic condition.
Dario Dongo
Cover art copyright © 2025 Dario Dongo (AI-assisted creation)
References
- Ahlström, M. G., Thyssen, J. P., Wennervaldt, M., Menné, T., & Johansen, J. D. (2019). Nickel allergy and allergic contact dermatitis: A clinical review of immunology, epidemiology, exposure, and treatment. Contact Dermatitis, 81(4), 227-241. https://doi.org/10.1111/cod.13327
- Commission Regulation (EU) 2024/1987 of 30 July 2024 amending Regulation (EU) 2023/915 as regards maximum levels of nickel in certain foodstuffs. http://data.europa.eu/eli/reg/2024/1987/oj
- Garg, S., Thyssen, J. P., Uter, W., Schnuch, A., Johansen, J. D., Menné, T., Belloni Fortina, A., Statham, B., & Gawkrodger, D. J. (2013). Nickel allergy following European Union regulation in Denmark, Germany, Italy and the U.K. British Journal of Dermatology, 169(4), 854-858. https://doi.org/10.1111/bjd.12556
- Lombardi, F., Fiasca, F., Minelli, M., Maio, D., Mattei, A., Vergallo, I., Cifone, M. G., Cinque, B., & Minelli, M. (2020). The effects of low-nickel diet combined with oral administration of selected probiotics on patients with systemic nickel allergy syndrome (SNAS) and gut dysbiosis. Nutrients, 12(4), 1040. https://doi.org/10.3390/nu12041040
- Rishor-Olney CR, Gnugnoli DM. Nickel Allergy. [Updated 2023 Jul 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557638/
- Silverberg, J. I., Patel, N., Warshaw, E. M., DeKoven, J. G., Belsito, D. V., Atwater, A. R., Taylor, J. S., Sasseville, D., Reeder, M. J., Houle, M. C., DeLeo, V. A., Maibach, H. I., Fowler Jr, J. F., Zug, K. A., Pratt, M. D., Yu, J., Mowad, C. M., Botto, N. C., & Adler, B. L. (2024). Patch testing with nickel, cobalt, and chromium in patients with suspected allergic contact dermatitis. Dermatitis, 35(2), 152-159. https://doi.org/10.1089/derm.2023.0139
- Silverberg, N. B., Pelletier, J. L., Jacob, S. E., & Schneider, L. C. (2020). Nickel allergic contact dermatitis: identification, treatment, and prevention. Pediatrics, 145(5), e20200628. https://doi.org/10.1542/peds.2020-0628
- Wennervaldt, M., Vaher, H., Ahlström, M. G., Bischofberger, N., Menné, T., Thyssen, J. P., Johansen, J. D., & Bonefeld, C. M. (2024). Subclinical immune responses to nickel in sensitized individuals: a dose-response study. Contact Dermatitis, 91(1), 1-10. https://doi.org/10.1111/cod.14549
Dario Dongo, lawyer and journalist, PhD in international food law, founder of WIISE (FARE - GIFT - Food Times) and Égalité.